October 14, 2021
Webinar: Trauma Considerations for Children and Adolescents
Written by Rachel Eddins
Posted in Trauma, Grief & Loss, Webinars and with tags: PTSD/Trauma, abuse, children

Trauma manifests in children and adolescents in many ways.
This webinar will cover signs and symptoms, treatments options, vicarious trauma, cultural considerations for trauma.
Facilitated by Maggie Burkett, LMSW.
Watch a replay of the presentation here.
Learn more about our trauma and PTSD treatment options.
Here is a transcription of the webinar:
Hello. This presentation is called Trauma Considerations for Children and Adolescents. I’m going to start by defining trauma, talking about what it is, some treatment treatments, some resources for parents and caregivers, and then some time for questions in case anyone has any.
What is “Trauma”?
Let’s start with just a broad definition of trauma. A traumatic event is one that poses a threat or serious injury or death to oneself or someone else. It usually elicits feelings of intense helplessness. There are Big T traumas. Then there are Little T traumas, which is not to say that some traumatic events are less important or less traumatizing than others. I think it can be very invalidating when we’ve experienced something that was for us horrific and for someone else to look at it and say: “Oh, that’s not really that big of a deal”.
I don’t want to focus too much on what a big trauma is and what a little trauma is, and I think it’s a little bit more helpful to think about as acute and chronic or complex.
Acute Trauma
Acute, does not mean that it’s not a big deal, but rather that it’s a single incident trauma. So we have someone who had a totally normal, wonderful life, and then one day they’re in a car accident in which someone in their car, one of their passengers dies. We would treat this as acute trauma. We’re treating the feelings that they have, the emotions, and what’s happening to their nervous system after there’s chronic trauma.
Chronic Trauma
Chronic trauma is something that happens repeatedly over a period of time. Typically, we see that associated with people that have survived intimate partner violence. They experience many different traumatic events over a long period of time.
Complex Trauma
Complex trauma is when there are two different traumatic events or two different traumatic actors happening simultaneously. We see that in kids that are growing up in poverty, although at home they might also be experiencing abuse. So a couple of different things going on at the same time.
We can also say that someone has experienced complex trauma or has complex PTSD when they’re an adult that experienced traumatic events in childhood and then separate traumatic events as an adult.
What causes trauma?
Probably all of us will experience a traumatic event in our lifetime. Life is dangerous and life has unsafe situations that can arise, but sometimes it can affect us long after the event, and it can have kind of outsize effects on us. It ends up being something that restores our memory of the events in a way that’s maladaptive so it ends up deeply impacting the rest of our life.
Something that I hear a lot from parents, caregivers, or teachers is about social media. We all experience traumatic events. However, I think social media has a lot to do with it. I saw this article on Slate last week that said how come everything on TikTok is a trauma response? And so I see people on TikTok saying all these things are trauma responses.
One of the things was wanting to keep your room clean. Well, that’s not necessarily a trauma response. I think that social media can be really good in that it seems to destigmatize trauma. People that have experienced trauma feel less alone. They feel like less of an outcast.
On the other hand, you get a lot of misinformation, like the example of cleaning your room as a trauma response. Of course, there are people who perhaps had an abusive caregiver that would force them to clean their room, and now they like to keep their room tidy. But in general, being an organized person doesn’t necessarily mean you’ve experienced the trauma. I think that with this kind of misinformation out there, you don’t realize that’s your anxiety.
Have I experienced trauma because I like to keep my room clean? No, not necessarily.
What Happens To The Brain When We Experience Trauma?
This is something that I like to talk about to all of my clients, whether they’re my youngest client at four years old, or older, so all across the lifespan. Obviously, there are many different parts of the brain. The brain is a complicated and beautiful machine, but for our purposes, we talk about trauma. We’re going to talk about two main parts of the brain.
I like to talk about the logical part of the brain, the part of the brain that controls executive-level functioning. The animal part of the brain is the first part of our brain to develop. It’s the oldest part of the brain, and it’s the part that controls our emotional responses, and it also controls our fight or flight response. It’s very powerful. And then as we get older, we develop a higher level of thinking. That part of the brain is the front part. The prefrontal cortex is the part that controls higher thinking, for example, what gives you the ability to write an essay or do higher-level mathematics.
Whenever we experience a trauma, our nervous system reacts very, very quickly, and it puts us in that fight or flight mode.
That part of our brain can actually shut down the logical part and kind of lets our animal part of the brain take over. You’re flooded with emotion, and you’re flooded with hormones like adrenaline in case you need to bite something else off or in case you need to run really fast.
When you think about it, humans had lots of danger coming at them all of the time. They had to be constantly on the defense or always ready to run away or always ready to fight, whatever the case may be.
But now, when we experience trauma, we get flooded with these hormones. When we are safe, we might know logically that we’re safe, but the animal part of the brain has shut down the logical part of the brain. It’s telling us that we need to run away.
That elevated status is where we have the animal part of the brain that’s taken over and shut down the logical part of the brain. That’s when we can see things like post-traumatic stress disorders start to occur. That’s when we realize that the trauma has affected us negatively. It’ll be something that happened six months or a year in the past, but we’re still showing symptoms as if the trauma had just happened.
Usually, when trauma has been maladaptively stored, we start using coping mechanisms that aren’t necessarily very healthy. Oftentimes we see trauma disorders cooccurring with substance use disorders and things like that because we’re all trying to calm our systems down after we’ve experienced this terrific event.
Cultural Considerations

Something I wanted to bring up towards the beginning of the presentation is cultural consideration. When I was in grad school, I often talk about cultural competency as kind of an afterthought. “Oh, yeah, these treatments might not work if you’re from different cultures.”
As I work with different clients and I’ve had the privilege of working with clients from many different cultures, I’ve noticed that our culture isn’t just limited to our race or ethnicity, but also to our religion or even our socioeconomic status.
Something that is traumatic to someone might not necessarily be traumatic to me. And all of that has to do with our culture. I think as practitioners or caregivers of children that have experienced the trauma, that’s something important to keep in mind. Especially I’ve noticed when the trauma is centered around death and grieving. The way that my family or my household or my particular community copes with loss, it’s going to look very different for other people.
How Does Trauma Impact Children/Adolescents/Young People?
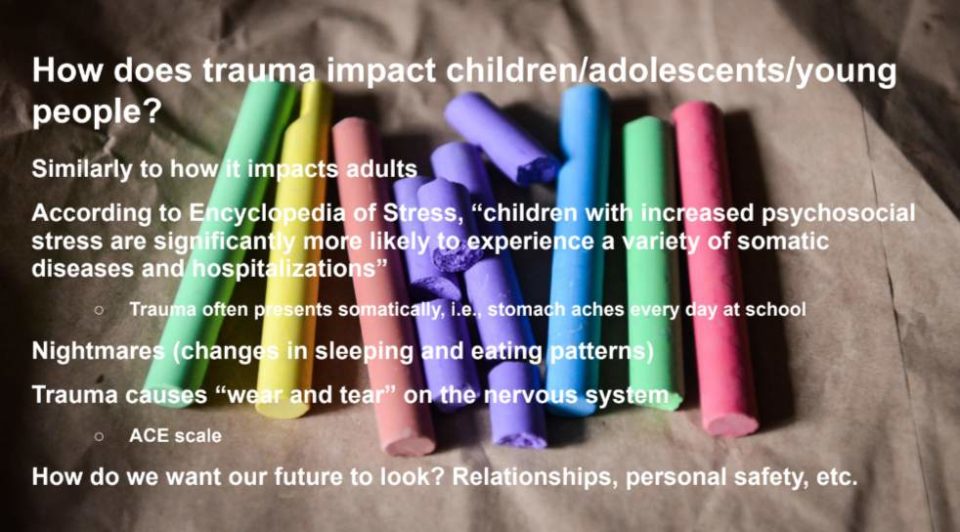
Let’s look at how trauma impacts children directly. As I mentioned before, it’s not going to be wildly different than how trauma impacts adults, but the way that they react to it’s going to be quite a bit different.
According to the Encyclopedia of Stress, “children with increased psychosocial stress are significantly more likely to experience a variety of somatic diseases and hospitalizations”.
Let’s talk about how trauma impacts children and adolescents, or tweens. The child can show signs every day when it’s time to go to school. If they’re complaining of a stomachache, I would think that there’s probably something going on that they’re not able to communicate. They’re not able to name the emotion, and they haven’t been able to process the trauma so it’s presenting as having a stomachache or a headache. But this is also something that can be experienced culturally. Sometimes I experience a fatty significance, like nervous attacks with my nerves. That’s kind of a somatic presentation of the traumatic event.
A really common symptom of a child that’s experienced trauma is nightmares, or more broadly speaking, changes in sleeping and eating patterns.
In fact, we often see that children regress after a traumatic event.
Maybe you have a five-year-old wanting to sleep in a parent’s bed, or four or three-year-olds start asking to wear diapers again long past the potty training phase and that is because they are feeling unsafe and they want to feel cared for. Remember feeling really cared for when they were a baby, so they’re regressing those behaviors.
However, for a lot of parents, it can be really frustrating. Just get out of the potty training phase and then the child wants to regress. That’s really difficult. Wants to start sharing a bed again and start sleeping dependency. But those kinds of changes in sleeping and eating and that regression is typically a result of problems. Children will often talk about bad dreams.
We can really see what a child is afraid of, and understand what they’ve suffered, what they’ve survived by what their nightmares are.
Trauma also causes undue wear and tear on the nervous system. People that score high on the ACE scale tend to be at a lot higher risk for physical and mental difficulty across the lifespan. So people who are clinically diagnosed as morbidly obese have very high ratings on the ACE Scale or the Adverse Childhood Experience Scale. This starts out with the family of origin.
Did you grow up in a single-parent home or did you have both parents present in the house? Were any of your parents incarcerated? Did your parents suffer from mental illness? And also it asks questions specifically about the child. When you were a child, were you often or very often made to feel unsafe in your home? Were you emotionally abused? Were you physically or sexually abused?
The higher someone is on the ACE field, the more likely they are to experience difficulties with their mental health, but also their physical health later on in life. Whenever we think about how trauma impacts children, we also must ask, what do we want their futures to look like?
When working with a child that has, for example, witnessed molesting by the parents, especially over a long period of time, they typically begin to understand that that’s how relationships work. That relationships are violent, that a loving relationship looks like this. Unless that child is able to process the trauma effectively, they might seek to replicate that relationship in their personal life as they get older.
Behaviors Associated With Children Who Have Experienced Trauma
Let’s talk about some behaviors that are associated with children who have experienced trauma. I’ve grouped them into two. The first one is challenging behaviors, which look like getting physically angry or physically fighting back, like hitting, punching, kicking, getting into fights at school, using curse words, and being generally disobedient. Oftentimes this accompanies an oppositional defiance disorder diagnosis, but not always.
The second group is fawning, people-pleasing behaviors. This can go too far in the opposite direction, and it can lead to things like eating disorders, or a child that self-harms. And both of these types of behavior are signs that a child is experiencing or going back to that fight or flight mode. They are not safe. They don’t feel safe. Rather, they don’t feel that they are safe.
Common Diagnosis and Misdiagnosis
Whenever a child that’s experienced a trauma comes in to receive treatment, they might be diagnosed with a bunch of different things. They could be diagnosed with acute stress disorder if the trauma has occurred recently, within the past month. If it’s happened longer than that, like six months ago, you’re going to traumatic stress disorder.
I mentioned complex PTSD earlier, but sometimes a child is misdiagnosed because a lot of the behaviors that I mentioned on the previous slide such as challenging behaviors or anxious people-pleasing behaviors can be misdiagnosed as oppositional, or as Attention Deficit Hyperactivity disorder.
This is also because kids that have experienced trauma sometimes can behave as if they’re not paying attention. Not always, of course, ADHD is a separate diagnosis, and some people exhibit those kinds of behaviors without ever having experienced the trauma. But sometimes it can present that way. So it’s really careful to avoid misdiagnosing and to avoid punishing a child for a behavior that’s associated with your child. So that’s something to look out for.
Treatments
I am an EMDR therapist and I also use Play Therapy. EMDR is fairly new, and it’s still kind of considered to be a newer treatment, but there is an evidence-based treatment. There’s a lot of evidence that supports EMDR’s use for treating trauma and even for treating children that have experienced trauma.
EMDR stands for Eye Movement Desensitisation and Reprocessing. It doesn’t have to be eye movements, but often times the therapist will ask the client to keep a dramatic event in mind and to follow our fingers what we classically say, and they move their eyes back and forth while keeping that treatment in mind. Ideally, it will decrease the level of disturbance that the client feels while recalling this trauma. So you always will remember it, it doesn’t remove it from your mind, but it’s just while talking about it. EMDR is an important treatment, especially because whenever we experience a trauma, we tend to tell ourselves a story about that trauma.
Whenever we experience an event in which we feel unsafe, we want to make sure we don’t feel that way again, so we take a lesson from it.
But sometimes, unfortunately, these lessons can be incorrect. For example, a child who is attacked by a stray dog experiences a traumatic event. The child might store this maladaptively as “I can’t be safe, or my parents don’t want to keep me safe” until they’re able to fully process the event. That might be something that they feel about themselves.
We can understand traumas that are more complex, such as being a survivor of sexual or physical violence. We might tell ourselves something wrong with us because we’ve experienced this or that, we don’t have value, we’re not worthy of love, and things like that. So whenever we’re looking for a treatment model for someone that has experienced trauma, it’s important that the treatment is addressing the story that the person has decided or is believing about themselves as a result of the trauma.
Play therapy is really helpful when treating trauma in children, usually between two and nine. But of course, it can vary depending on a child’s developmental age. Play therapy can be extremely effective because in the playroom there are all sorts of toys but nothing electronic, and it allows the child to play through the situation of the traumatic event itself.
Children learn through playing. That’s how they learn, and also how they communicate.
There’s a world-renowned play therapist who often gives the example of a child who saw his brother drowning in the house. He comes into the play therapy session every week and gets out the baby doll and put the baby doll in the sink and pretends to be filling the sink with water. And it would repeat that action until they no longer felt those high levels of disturbance associated with the trauma. Of course, it will still be a distressing event. There’s no way around it.
Sometimes what the children need in order to heal is to feel that they ended up making the right decision, whether it’s saving the baby but they are harmed, or whether it’s telling an adult right away that the baby is underwater or something like that.
We can also use dialectical behavior therapy to treat trauma. Exposure therapy was one of the older models of therapy, meaning that we’ve used it for a long time.
Exposure therapy, especially with children, can sometimes be retraumatizing and it can sometimes do more harm than good.
There’s also a higher trauma to the practitioner whenever they’re using exposure therapy. So there are pros and cons associated with each of these treatment models. Let’s look at what parents and caregivers can do to support treatment at their home or at school. One of the biggest factors in being able to predict a successful outcome of treatment for a child or adolescent experiencing trauma is whether or not they’re able to live a stable, healthy lifestyle. So this does involve being able to go outside and get fresh air, eating a balanced diet, and keeping to a routine. This is something that I see a lot of parents and caregivers struggling with.
After a child has experienced trauma oftentimes parents want to allow them to kind of get special treatments. I think that’s a very natural impulse. The child has been through a lot, and you want to kind of be less hard on them. This could end up backfiring and it can end up being harmful because having a predictable routine and being able to predict parents’ reactions to behaviors is one of the main ways that a child can establish feelings of safety.
If one experiences trauma and then they go home and they talk back or something that is a rule in the household. They break a rule in the household and their parents want to in the past, the child is going to feel everything has changed. Up is down, and down is up. You can’t predict what’s going to happen, and that’s going to contribute to those feelings of being unsafe.
Something that’s a little bit controversial is the use of psychopharmaceuticals.
It doesn’t necessarily have to be controversial. There’s a large body of evidence that supports the use of psychopharmaceuticals in treating trauma. Children with a history of trauma are wary of their use. There are a lot of stigmas associated with taking medications, but medication combined with therapy, combined with living a healthy, balanced lifestyle, a child tends to have a very good indication that they’ll be able to move through this traumatic event and be able to process it successfully.
Something that I should have listed here, but I didn’t is also TF-CBT. There’s a high body of evidence that supports the use of TF-CBT in patients that have experienced trauma. So that’s going to be your cognitive behavioral therapy, in which the practitioner explores the relationship between someone’s thoughts, feelings, and behaviors while applying a trauma-informed lens. This tends to be helpful for patients that tend to enjoy talking, and that need to go to a therapist and really explore and sort out their problems.
As opposed to EMDR, which is a more scripted, less flexible protocol, where you’re focusing directly on the traumatic event and how it made you feel, TF-CBT tends to take a little bit longer, but it allows you to really go deep, for lack of a better term, on all the things that they might be experiencing.
Coping Mechanisms
Let’s talk about some coping mechanisms that you can use outside of the treatment room.
Hot Chocolate
So something that I really like to use is a visual that I like to use called smelling and cooling hot chocolate. So with an adult, I might say taking really deep inhales through your nose and exhaling through your mouth. But for a kid, it’s a good idea to use something that they have maybe a positive association with and get a really strong mental image of. If you’re holding hot chocolate, or a glass of water and encouraging the child to pretend that they’re smelling. So taking a really deep, profound inhale through the nose and then cooling it so exhaling through the mouth.
That also helps to get a mental image of a cup of hot chocolate. And that helps to allow the animal part of the brain to kind of step back a little bit since it’s really elevated and allows the logical part to kind of step in. Because we’re asking the child to imagine holding a cup of hot chocolate and your emotions are really high and you’re just dysregulated imagining something else or being able to have kind of a sensory experience of something else is really helpful to re-regulate.
A Calm Down Space
I see in a lot of classrooms teachers utilizing a calm down space. I think that’s a really great idea. A place that a child can go that they have positive associations with, a place for them to kind of gather their thoughts before they kind of move back into the classroom environment. I think it’s also totally appropriate to have a place that’s designated for that in your home, whether it’s a nook in the living room or something like that. But a place where a child knows that they can go when they just need to take a breather and maybe that can signify to the rest of the family. “Johnny needs a second to calm down. So we’re going to let him calm down whenever he’s ready to rejoin the family or rejoin what everybody else is doing, he’s welcome to do so.”
Earlier I stated the importance of maintaining routine rules and expectations in the home or in the classroom after a child has experienced a trauma. It’s also really important before we enforce the rule or certainly before we decide that punishment needs to take place, we need to build that connection first. Recognize that a child who’s behaving really disruptively, who’s hitting and kicking, it’s important that we take a second and connect with them.
Just acknowledge that you see them and you notice that they’re in pain and you’re going to kind of sit with them in that space of pain before you correct the behavior.
This is really helpful because it helps the child name the emotion. There’s kind of a phrase in the therapy for children that says: Name it to tame it. So if we’re able to say:
“You know what? I’m being angry right now.”
Step outside of the animal mind and kind of let our logical mind step in for a second. Recognize what we’re experiencing, and then it’s a little bit easier to decrease from the dysregulation to a place where feeling calmer. I’m a big fan, especially when working with teenagers, of using the 5,4,3,2,1 senses, so that whenever we recognize that we’re in. The first step would be to recognize that we’re in a heightened state, that we’re from a place of emotion or a place of intense fear, and use our senses to help us orient to the present and help us feel safer. So that starts with five:
- 5 – things that you can see
- 4 – things that you can touch
- 3 – things that you can hear
- 2 – things you can smell
- 1 – thing you can taste.
So any room that they’re in, this can be done anywhere, you can do it in the classroom, you can remember to do it when you’re in a car when you’re at home. And it obviously doesn’t require any kind of props, but it really allows us to orient to the present and thus feel that we can be safe.
We’re not kind of trapped in the memory of the traumatic event.
It’s also important, even though it feels logical, like whenever it might feel like that’s a natural time and place to kind of teach a lesson, to kind of say, “Oh, you know what? I think that it would be a really good idea if we learn from this and do X, Y, and Z.” But whenever we’re in a heightened state, if I’m very upset, if I’m very stressed out, that’s not really the place where I can learn. That’s not really the place that I learned from. My emotions are running high, and I’m not able to take a step back.
So the first thing to do before the lessons, before the correction again, is going to be to use mindfulness, take a deep breath, calm down a little bit, make that connection, and name the emotion before we move on to how we can use this as a learning opportunity.
Ask For Help
So when I’m working with parents or caregivers, questions that they ask frequently are how soon will it get better or how long is this going to take? It’s perfectly natural to want to know that. We want to make sure our children, our loved ones, are feeling better as soon as possible.
Unfortunately, the answer is it depends. It depends on the level of stability in the child or teenager’s life at the moment, it depends on whether they’re able to feel safe. It depends on whether or not they are surrounded by memories of the traumatic event through the traumatic person are better known as triggers. Depends on how often they’re exposed to triggers.
The best way to support the therapeutic process is to help the child or teenager maintain that healthy lifestyle, making sure that they’re getting adequate sleep, that they’re able to get outside, get some exercise, and appropriate amount, make sure that they’re eating well.
How do we set expectations and milestones without pushing too hard?
That’s a really good question. Sometimes parents who are incredible parents may be pushing the child a little bit too far. This is being described as a kind of toxic positivity, and that’s a very difficult conversation to have. But if the child is feeling down about the trauma and they want to talk to the parent about it and the parent just says: “Oh, you need to just put that behind you. You need to get past it. You stop thinking about it so much, you need to move forward.”
The child, unfortunately, is going to feel pretty invalidated by that. It’s still a big part of their life. There are better results if you allow yourself again to sit with a child, or a teenager in that space, to sit with them in the pain, the bad feeling, the yucky feeling.
Trauma can be so isolating. You can really feel like you’re the only person in the world that’s gone through this.
No one feels worse than you do, especially when you’re a child or you’re a teenager. So having someone that you love and trust, sitting with you and sharing that and kind of shouldering that burden with you for a little bit, it can really change your world. It can be exactly what you need.
In Texas, any adult that even suspects that a child, teenager, or person under 18 years old is being abused or exploited is required by law to report it to CPS. You can report it online, or you can report it by phone. That’s something that we need to remember. I think a lot of times people think that you might be the only person that does your fault and that can really change someone’s life for the better by making that report.
Resources for Parents, Caregivers, Teachers, Etc.
https://www.apa.org/topics/trauma
https://mmhpi.org/work/trauma-grief-center/
- A Terrible Thing Happened: A Story for Children Who Have Witnessed Violence or Trauma, Margaret M. Holmes
- Children and Trauma: A Guide for Parents and Caregivers, Cynthia Monahon
- Trauma Through a Child’s Eyes: Awakening the Ordinary Miracle of Healing, Peter A. Levine, PhD.
- “What is trauma? How do we help children who experience trauma?” by DeveloPlay on Youtube: https://www.youtube.com/watch?v=QlNBPPrjIE8
I also wanted to make sure I had some time to go over some resources that people can use. I’m a big fan of using books. And there’s a really wonderful book for children called “A Terrible Thing Happened: A Story for Children Who Have Witnessed Violence or Trauma”. It’s by Margaret M. Holmes.
And it’s for kids who witness violence or trauma. And then for books for parents or care, “Trauma Through a Child’s Eyes” by Peter Levine, who has written many books starting in the 1970s about trauma and trauma treatment.
You can also find really helpful YouTube videos.
However, just like everything on the Internet, it’s really important to be able to identify the source who’s putting out the YouTube videos, because there can be, unfortunately, a lot of misinformation and bad information out there.
But this is a video by an Institute that treats children who have experienced trauma. Typically, I would say if you’re looking for a YouTube video, look at who put out the video, who uploaded it, and if they’re associated with an organization or with a private practice, even then their information will probably be a lot better than someone who’s got kind of like a silly username. It doesn’t have any other helpful information in the description.
There are, of course, other websites that you can use. In Houston, the Children’s Assessment Center is the absolute best resource for children and sexual abuse. Anyone can go at any age, actually, even adults who had experienced sexual abuse as a child. You can go there for therapy, or for family advocates. It’s a really wonderful place. Both places have free resources and they are for children and families that have experienced grief. They do free therapy, and they also have a lot of events.
It can be really helpful and powerful for children and adolescents to read books containing the same things that they have because trauma can be very isolating.
There’s also the Trauma & Grief Center in Houston. They used to be part of Texas Children’s Hospital, but now they are part of a different organization. This link here has a ton of free resources. They have webinars and literature available for parents and caregivers that are looking to learn how to work with their children or adolescents that have experienced trauma.
There’s the National Center for Traumatic Stress in Children. There’s also the American Psychological Association, a great page where they talk about how to talk about traumatic events with your child.
About the Presenter
I realized I did not properly introduce myself. I’m Maggie Burkett Digilova. I am a therapist and I worked for a long time doing social work in community outreach before I got my master’s, I was actually working in Houston and Independent School District. I taught the language in first grade, so Spanish and English. And that’s when I really became very interested in how traumatic events can impact cognition.
All of the children that I worked with either themselves were immigrants from Central America, or their parents experienced significant trauma in early childhood and I decided that I really wanted to get my master’s and work with this population and so I’m proud to say that that is what I’ve done ever since.
Thank you and I’d love to hear from you if you have any questions or any feedback or if you might like to work together and collaborate. I really think that when it comes to trauma treatment the human capacity to harm one another is vast. I think things will only get better if we work together so please don’t be shy to reach out and look forward to hearing from working with you and thank you all for the opportunity.
Grounding & Self Soothing
Get instant access to your free ebook.